Summary
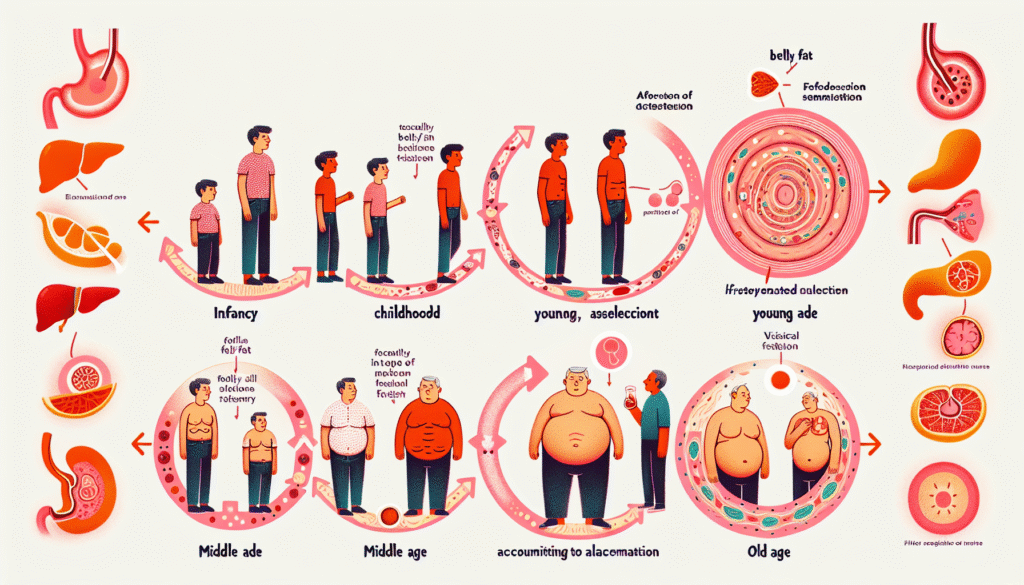
Recent research reveals that aging activates a newly identified type of stem cell that efficiently generates fat cells, offering insight into why belly fat commonly increases during middle age. Scientists discovered that aging triggers adipocyte progenitor cells (APCs) to transition into age-specific committed preadipocytes (CP-As), which aggressively produce fat.
A signaling pathway known as LIFR was found to be responsible for this surge in fat-cell development. These insights may pave the way for therapies targeting CP-As to help curb age-related fat accumulation and metabolic diseases.
Key Facts
New Fat-Making Cells: Aging leads to the appearance of CP-A cells that produce a significant number of fat cells.
Critical Pathway Identified: The LIFR signaling pathway is essential in driving the formation of fat cells, particularly in middle age.
Potential Therapy Target: Disabling CP-As may reduce age-related belly fat and potentially increase lifespan.
Source: City of Hope
It’s widely recognized that waistlines often grow during middle age—but the issue extends beyond appearance. Belly fat contributes to accelerated aging and reduced metabolism, heightening the risk of diabetes, cardiovascular issues, and other long-term health concerns.
However, the biological mechanisms behind this midsection expansion have been largely unclear—until now.
Groundbreaking preclinical research from City of Hope—one of the U.S.’s largest and most advanced institutions for cancer and diabetes research—has identified the specific cells behind this age-related fat gain.
Published in Science, this discovery provides a new potential therapeutic target for tackling belly fat and promoting a longer, healthier life.
“People often lose muscle and gain body fat as they age—even when their body weight remains the same,” said Qiong (Annabel) Wang, Ph.D., the study’s co-corresponding author and an associate professor of molecular and cellular endocrinology at City of Hope’s Arthur Riggs Diabetes & Metabolism Research Institute.
“We discovered aging triggers the arrival of a new type of adult stem cell and enhances the body’s massive production of new fat cells, especially around the belly.”
In partnership with Xia Yang, Ph.D., from UCLA, researchers ran mouse-based experiments later validated using human cells. The study centered on white adipose tissue (WAT), the fat tissue responsible for weight gain linked to aging.
While it’s known that fat cells enlarge with age, the team hypothesized that WAT might also expand due to the creation of new fat cells—implying virtually unlimited growth potential.
To test this, researchers investigated APCs—stem cells in WAT that mature into fat cells. They transplanted APCs from both young and older mice into a new group of young mice. Remarkably, APCs from older mice generated a large quantity of new fat cells.
When the reverse experiment was conducted—transplanting young APCs into older mice—few new fat cells were formed. This suggested that older APCs are independently primed to produce fat cells, regardless of their environment.
Using single-cell RNA sequencing, the team analyzed APC gene activity in both age groups. In younger mice, the APCs were mostly dormant. But in middle-aged mice, they were highly active, creating a surge of new fat cells.
“While most adult stem cells’ capacity to grow wanes with age, the opposite holds true with APCs — aging unlocks these cells’ power to evolve and spread,” said Adolfo Garcia-Ocana, Ph.D., the Ruth B. & Robert K. Lanman Endowed Chair in Gene Regulation & Drug Discovery Research and chair of the Department of Molecular & Cellular Endocrinology at City of Hope.
“This is the first evidence that our bellies expand with age due to the APCs’ high output of new fat cells.”
As aging progresses, APCs develop into a novel category of stem cells called committed preadipocytes, age-specific (CP-As), which are highly active in generating fat—especially in middle age.
The LIFR (leukemia inhibitory factor receptor) signaling pathway was pinpointed as the key driver that encourages CP-A cells to multiply and form fat cells.
“We discovered that the body’s fat-making process is driven by LIFR. While young mice don’t require this signal to make fat, older mice do,” explained Wang.
“Our research indicates that LIFR plays a crucial role in triggering CP-As to create new fat cells and expand belly fat in older mice.”
Using single-cell RNA sequencing on human tissue samples from different age groups, the researchers also identified similar CP-A cells in people. These CP-As were significantly more prevalent in middle-aged individuals and showed a strong ability to produce fat cells.
“Our findings highlight the importance of controlling new fat-cell formation to address age-related obesity,” said Wang.
“Understanding the role of CP-As in metabolic disorders and how these cells emerge during aging could lead to new medical solutions for reducing belly fat and improving health and longevity.”
Future investigations will focus on monitoring CP-A cell behavior in animals, studying them in human tissue, and designing interventions that inhibit or eliminate them to combat age-related fat accumulation.
This study’s first authors are Guan Wang, Ph.D., from City of Hope, and Gaoyan Li, Ph.D., from UCLA.